Tuesday 10 May 2016
Friday 6 May 2016
Tuesday 3 May 2016
ANKLE AND WRIST BLOCK





Both components of the sciatic nerve, common peroneal (CP) and tibial (T) nerves diverge from each other at the popliteal fossa. Lateral and medial gastrocne- mius muscles (GN) are also shown.

The sural nerve is shown behind the lateral malleolus.
 .
. 


- Saphenous n
- Blocks postero-medial part of dorsum of foot
- Superficial infiltration around long saphenous vein anterosuperior to medial malleolus
- Tibial n
- Needle entry medial to Achilles tendon or lateral to posterior tibial artery at upper border of medial malleolus
- Determine depth with paraesthesia, nerve stimulator or 1 cm superficial to tibia
- Alternatively infiltration either side of artery behind medial malleolus
- Blocks sole, plantar surface of digits
- Deep peroneal n
- Needle entry between extensor hallucis longus and tibialis anterior tendons or lateral to anterior tibial artery
- Blocks first web space and short toe extensors
- Superficial peroneal n
- Superficial infiltration from lateral border of tibia to upper part of lateral malleolus
- Blocks dorsum of foot and toes except first web space
- Sural n
- Superficial infiltration from Achilles tendon to lateral malleolus
- Blocks lateral side of foot and fifth digit





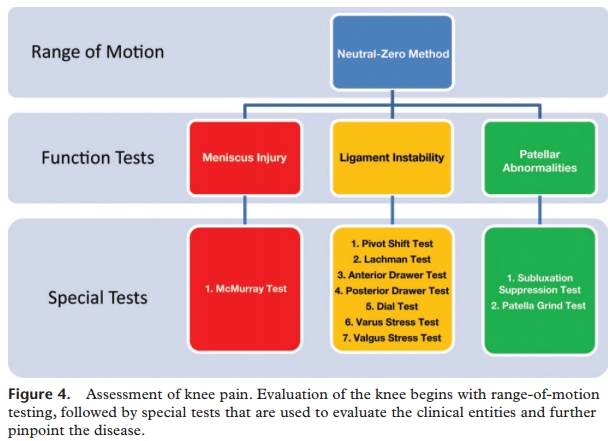
Knee Pain Special Test

The physician begins by comparing the painful knee with the asymptomatic knee and inspecting the injured knee for erythema, swelling, bruising, and discoloration. The musculature should be symmetric bilaterally.
The knee is then palpated and checked for pain, warmth, and effusion. Point tenderness should be sought, particularly at the patella, tibial tubercle, patellar tendon, quadriceps tendon, anterolateral and anteromedial joint line, medial joint line, and lateral joint line.

LACHMAN TEST

The Lachman test is another means of assessing the integrity of the anterior cruciate ligament (Figure 3).7 The test is performed with the patient in a supine position and the injured knee flexed to 30 degrees. The physician stabilizes the distal femur with one hand, grasps the proximal tibia in the other hand, and then attempts to sublux the tibia anteriorly. Lack of a clear end point indicates a positive Lachman test.
ANTERIOR AND POSTERIOR DRAWER TEST
VARUS AND VALGUS STRESS TEST
The valgus stress test is performed with the patient's leg slightly abducted. The physician places one hand at the lateral aspect of the knee joint and the other hand at the medial aspect of the distal tibia. Next, valgus stress is applied to the knee at both zero degrees (full extension) and 30 degrees of flexion (Figure 4)7. With the knee at zero degrees (i.e., in full extension), the posterior cruciate ligament and the articulation of the femoral condyles with the tibial plateau should stabilize the knee; with the knee at 30 degrees of flexion, application of valgus stress assesses the laxity or integrity of the medial collateral ligament.

EMERGENCIES IN ORTHOPAEDICS
1. UNSTABLE PELVIC FRACTURES
Initial Evaluation
-----ATLS protocol : ABCDE's
-----1st & 2nd Survey
Open Pelvic Fractures
-----Perineal Laceration
-----Vaginal Injuries
-----Rectal Injuries
Associated Injuries
----MAjor Blood Vessel : Internal Iliac/Branches , Pelvic Vein
----Neurological Compromise: Lumbosacral plexus, Cauda Equina
----Lower GI tract
----Lower GU tract
Radiographic
---->2.5 displacement of symphysis
---->5mm displacement of SI complex
----Presence of posterior fracture gap
----Avulsion fractue
CLASSIFICATION
A; stable
B: rotationally unstable, vertically stable
C: rotationally and vertically unstable
2. OPEN FRACTURES
CLASSIFICATION
----Gustillo-Anderson
In ED
----Appropriate AB
----TEtanus status
----Realign extremity and splint
3. COMPARTMENT SYNDROME
Compression/Constriction of vessels, nerves and muscles in closed fascial compartment resulting in
-> decreased perfusion
->ischemia
->cell death
Diagnosis: Pain, Pallor, Paresthesia, Pulselessness, Paralysis
Measurement
----Intracompartment pressure >30mmHg
----Diff between dias and intracompartment <30mmHG
- hemodynamic instability
- GU injury
- Nerve injury
- Mortality
Initial Evaluation
-----ATLS protocol : ABCDE's
-----1st & 2nd Survey
Open Pelvic Fractures
-----Perineal Laceration
-----Vaginal Injuries
-----Rectal Injuries
Associated Injuries
----MAjor Blood Vessel : Internal Iliac/Branches , Pelvic Vein
----Neurological Compromise: Lumbosacral plexus, Cauda Equina
----Lower GI tract
----Lower GU tract
Radiographic
---->2.5 displacement of symphysis
---->5mm displacement of SI complex
----Presence of posterior fracture gap
----Avulsion fractue
CLASSIFICATION
A; stable
B: rotationally unstable, vertically stable
C: rotationally and vertically unstable
2. OPEN FRACTURES
CLASSIFICATION
----Gustillo-Anderson
In ED
----Appropriate AB
----TEtanus status
----Realign extremity and splint
3. COMPARTMENT SYNDROME
Compression/Constriction of vessels, nerves and muscles in closed fascial compartment resulting in
-> decreased perfusion
->ischemia
->cell death
Diagnosis: Pain, Pallor, Paresthesia, Pulselessness, Paralysis
Measurement
----Intracompartment pressure >30mmHg
----Diff between dias and intracompartment <30mmHG
Acromio-Clavicular Injury

| Presentation | ||||
|
Subscribe to:
Posts (Atom)